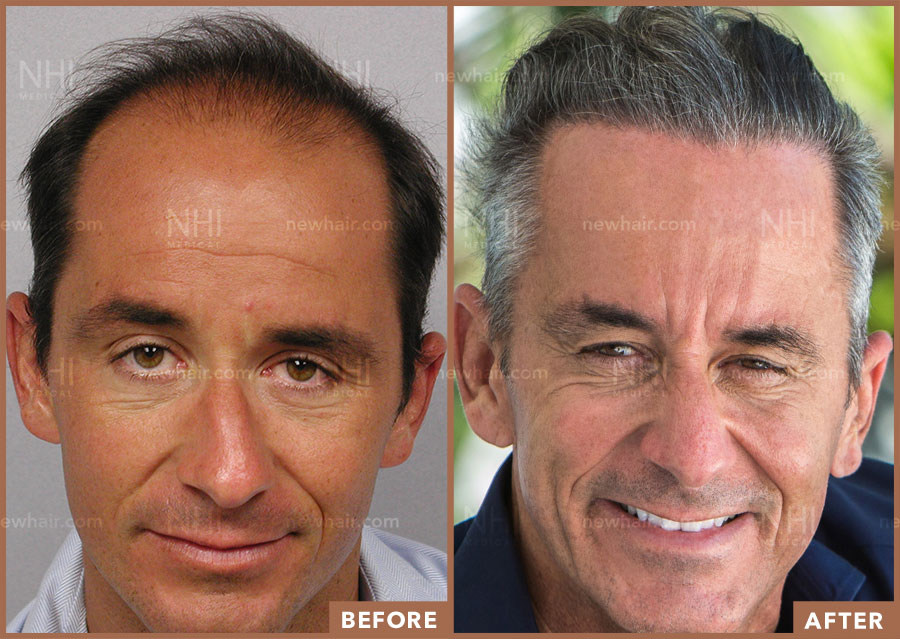
Follicular Unit Excision
The most advanced hair transplant method for hair loss in Los Angeles
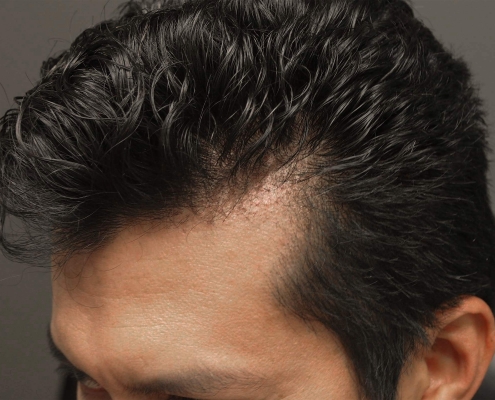
Follicular Unit Excision (FUE) is a cutting-edge hair transplant procedure that allows you to wear your hair long or incredibly short without the fear of showing a linear scar. The FUE technique can be used for hair transplants, hairline lowering, eyebrow transplants, beard transplants, and scar revisions.